Contents
Heart attacks, recognized as a leading cause of death worldwide, represent critical medical emergencies that necessitate immediate attention.
Gaining a comprehensive understanding of the nature, causes, symptoms, and survival odds associated with heart attacks can give the power to individuals to engage in preventive measures.
One crucial question to consider is – What are the odds of surviving a heart attack?
This article delineates what constitutes a heart attack, identifies the associated risk factors, and discusses the vital signs that should be monitored.
Additionally, it emphasizes the importance of diagnostic procedures, treatment options, and lifestyle modifications that can mitigate one’s risk.
By equipping oneself with this knowledge, individuals can take proactive steps to protect their heart health and enhance overall well-being.
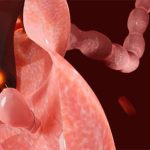
What is a heart attack?
A heart attack, medically referred to as a myocardial infarction, occurs when there is a significant reduction in blood flow to the heart muscle, usually resulting from a blockage in one or more coronary arteries.
This blockage can lead to cardiac arrest, a critical condition that necessitates immediate medical intervention.
Heart attacks represent a leading cause of morbidity and mortality on a global scale and are primarily associated with heart disease, which includes a range of cardiovascular disorders.
What causes a heart attack?
Heart attacks are predominantly caused by coronary artery disease (CAD), which occurs due to the accumulation of plaque within the arteries, thereby restricting blood flow to the heart.
Several risk factors, including lifestyle choices such as smoking, obesity, diabetes, hypertension, and elevated cholesterol levels, significantly contribute to the progression of CAD.
Furthermore, additional factors such as age and gender may also influence an individual’s susceptibility to experiencing a heart attack.
What are the risk factors for a heart attack?

Numerous risk factors can significantly increase the likelihood of experiencing a heart attack, including personal health history, family health history, and individual lifestyle choices.
Conditions such as obesity, smoking, diabetes, hypertension, and high cholesterol markedly elevate these risks. Understanding the impact of age and gender on susceptibility can facilitate effective risk assessment and the development of preventive strategies.
For instance, research indicates that individuals with a body mass index (BMI) exceeding 30 face a considerably heightened risk, with obesity contributing to nearly 300,000 deaths annually in the United States alone.
Smoking is a significant risk factor, with smokers experiencing a 70% increased likelihood of developing heart disease compared to non-smokers.
Similarly, diabetes plays a critical role, as approximately 68% of adults with this condition die from heart-related issues.
Hypertension, often referred to as the “silent killer,” affects nearly 45% of adults in the U.S. and is directly correlated with an increased risk of heart attack.
Additionally, the importance of familial factors cannot be understated – individuals with a family history of heart disease are two to three times more likely to experience similar health issues, irrespective of their personal lifestyle choices. This raises an important question: What are the odds of surviving a heart attack for individuals with these risk factors?
What are the symptoms of a heart attack?
The symptoms of a heart attack can vary significantly among individuals – however, they typically include chest pain, shortness of breath, nausea, and discomfort in the arms, back, neck, or jaw.
Early recognition of these symptoms is crucial for timely medical intervention, as prompt treatment can enhance outcomes and mitigate the risk of complications associated with myocardial infarction.
How long do heart attack symptoms last?
The duration of heart attack symptoms can vary significantly, ranging from a few minutes to several hours, and may present in an unpredictable manner.
Understanding this variability is essential for individuals and their families, as it highlights the critical importance of seeking immediate medical attention and emergency response when symptoms occur – timely intervention can markedly improve survival rates.
Several factors influence the duration of these symptoms, including the individual’s overall health, the presence of pre-existing medical conditions, and the promptness of medical intervention.
Common symptoms such as chest pain, shortness of breath, or discomfort in other areas of the upper body may signify a serious condition that requires immediate attention.
In certain situations, the availability of emergency medical services and the rapidity with which paramedics can provide treatments, such as defibrillation or medication, can have a significant impact on patient outcomes.
Early recognition of the signs and swift action can not only mitigate symptoms but also prevent more extensive damage to the heart muscle.
What should you do if you have symptoms of a heart attack?
If you or someone you know displays symptoms indicative of a heart attack, immediate action is imperative.
It is crucial to contact emergency services without delay and initiate first aid measures, including the administration of CPR if necessary.
This prompt response can help maintain blood flow and enhance the chances of survival until professional medical assistance is available, underscoring the life-saving potential of utilizing a defibrillator if one is accessible.
Recognizing the signs of a heart attack, such as chest pain, shortness of breath, or discomfort in other areas like the arms or back, is of utmost importance.
After contacting emergency services, it is essential to ensure that the individual remains calm and is positioned comfortably, either seated or lying down.
In the event the individual is unresponsive, commence CPR immediately at a steady rate of 100-120 compressions per minute, being mindful to employ the correct technique to provide effective assistance.
This cycle of immediate action and proper first aid can significantly improve the likelihood of a favorable outcome.
It is important to remember that your prompt actions are not only beneficial but often critical in saving a life and facilitating timely medical treatment.
What are the odds of surviving a heart attack?

The likelihood of surviving a heart attack can differ considerably based on various factors, such as the promptness of medical intervention, the specific type of heart attack, and the individual’s overall health status.
Research indicates that timely intervention substantially improves patient outcomes, underscoring the importance of awareness regarding risk factors and symptoms to enhance survival rates associated with myocardial infarction.
What factors affect the survival rate of a heart attack?
Several factors influence the survival rate following a heart attack, including the promptness of emergency response, access to healthcare, and the quality of medical treatment administered.
Individual characteristics such as age, gender, medical history, and lifestyle choices also significantly impact the prognosis after a myocardial infarction. In this context, many people wonder: what are the odds of surviving a heart attack?
Timely intervention is essential – expedited emergency response times can markedly enhance survival probabilities by minimizing the duration of oxygen deprivation to the heart.
Access to high-quality healthcare facilities is equally crucial – individuals residing in urban areas generally benefit from superior resources and specialized care compared to those in rural locations.
Recent advancements in medical technology and treatment strategies, including the utilization of thrombolytics and catheter-based interventions, have shown promise in improving patient outcomes.
Additionally, personal health factors, such as the presence of comorbidities such as diabetes and hypertension, can complicate recovery, underscoring the necessity for effective management of pre-existing health conditions.
Post-event lifestyle modifications, including the adoption of a heart-healthy diet and regular physical activity, are vital in fostering long-term survival and enhancing overall quality of life.
What is the average survival rate for a heart attack?
The average survival rate for individuals experiencing a heart attack has improved significantly over the years, thanks to advancements in cardiac care and medical treatment.
Current statistics indicate a survival rate of approximately 90% when prompt intervention is provided.
These figures underscore the critical importance of rapid response and effective medical care in enhancing survival probabilities for individuals undergoing a myocardial infarction.
Historical data reveal that survival rates were considerably lower just two decades ago, often around 70%.
This notable progress can be attributed to improved emergency response protocols, the development of new medications, and innovative surgical techniques that emphasize the need for immediate medical attention.
Furthermore, the emphasis on educating the public about heart attack symptoms and the importance of contacting emergency services has also been instrumental in improving outcomes.
As these statistics illustrate, timely access to healthcare is essential – even a matter of minutes can profoundly impact the outcomes for individuals facing a cardiac emergency. These changes reflect an improved understanding of what are the odds of surviving a heart attack in the modern healthcare landscape.
How is a heart attack diagnosed and treated?
Diagnosing a heart attack generally requires a comprehensive approach that includes clinical evaluation, diagnostic tests, and imaging studies to assess the condition of the heart and its blood flow.
Common diagnostic tools utilized in this process consist of an electrocardiogram (ECG), blood tests for cardiac biomarkers, and imaging techniques such as echocardiograms.
These methods work in conjunction to provide critical information that guides the selection of appropriate medical treatment options tailored to the patient’s specific needs.
What tests are used to diagnose a heart attack?
Several diagnostic tests are employed to ascertain the occurrence of a heart attack, with the electrocardiogram (ECG) being one of the primary tools for evaluating cardiac activity.
Additional tests, including blood assays for cardiac enzymes, echocardiograms, and imaging techniques such as angiography, are instrumental in assessing the extent of myocardial damage and determining necessary interventions, such as angioplasty or stent placement.
These diagnostic methodologies are essential for the timely and accurate identification of myocardial infarction.
The ECG captures the electrical activity of the heart, facilitating the identification of arrhythmias and ischemic changes in real time.
Blood tests, particularly those measuring troponin levels, offer valuable insights into myocardial damage, while echocardiograms leverage sound waves to generate detailed images, thereby aiding in the evaluation of cardiac function.
Angiography, frequently conducted in conjunction with catheterization, permits direct visualization of the coronary arteries, allowing for an assessment of the severity of blockages and the identification of the most appropriate treatment options.
Each of these tests plays a significant role in informing clinical decisions and enhancing patient outcomes.
What are the treatment options for a heart attack?
Treatment options for heart attacks vary significantly based on the severity of the condition, ranging from medication management to more invasive procedures.
Medical interventions may encompass the administration of thrombolytic agents, coronary angioplasty, stent placement, or, in more severe cases, coronary bypass surgery. Additionally, cardiac rehabilitation programs are essential for supporting recovery and promoting long-term heart health.
Timely intervention is critical when a patient experiences a heart attack. In instances of minor blockages or initial symptoms, pharmacological treatments such as antiplatelet agents or beta-blockers may sufficiently restore blood flow and manage symptoms.
For more significant blockages, coronary angioplasty is often the preferred intervention, utilizing a small balloon to open the affected arteries. Stent placement may be concurrently performed to maintain arterial patency.
In severe cases where extensive artery blockage is present, coronary bypass surgery may be indicated to redirect blood flow around the obstructed artery.
Following initial treatment, it is generally recommended that patients engage in cardiac rehabilitation to enhance overall heart health, facilitate recovery, and mitigate the risk of future cardiovascular events.
How can you prevent a heart attack?

Preventing a heart attack requires a comprehensive strategy that encompasses the adoption of heart-healthy lifestyle modifications and a thorough understanding of risk reduction strategies.
Essential preventive measures include:
- Maintaining a balanced diet;
- Engaging in regular physical activity;
- Managing stress levels;
- Abstaining from tobacco use.
Implementing these practices can significantly reduce the risk of developing heart disease and experiencing a myocardial infarction.
What lifestyle changes can help prevent a heart attack?
Implementing specific lifestyle changes is essential for the prevention of heart attacks, with particular emphasis on dietary improvements, regular physical activity, and effective stress management techniques.
By making informed decisions that prioritize cardiovascular health, individuals can significantly reduce their risk.
A heart-healthy diet, for instance, not only limits the consumption of saturated fats and sugars but also includes an abundance of fruits, vegetables, whole grains, and lean proteins, all of which provide essential nutrients necessary for overall well-being.
In conjunction with this dietary approach, engaging in a regular exercise regimen – such as brisk walking or cycling – can help maintain a healthy weight and manage hypertension, both of which are critical risk factors for heart disease.
Moreover, incorporating stress management techniques, such as mindfulness, yoga, or deep-breathing exercises, can assist in lowering cortisol levels, thereby reducing stress on the heart.
These interconnected strategies collectively contribute to establishing a robust defense against heart attacks. Nonetheless, understanding “what are the odds of surviving a heart attack” can provide additional motivation for adhering to these preventive measures and fostering a healthier lifestyle.
What medical treatments can help prevent a heart attack?
Medical treatments can play a significant role in preventing heart attacks, particularly for individuals who are at higher risk.
Medications such as statins, anticoagulants, and antihypertensive agents are effective in managing cholesterol levels, blood pressure, and overall cardiovascular health.
Additionally, regular health screenings and consultations with healthcare professionals are essential for ongoing risk assessment and the development of prevention strategies.
Alongside these pharmacological interventions, lifestyle modifications are critical to maintaining heart health. This includes adherence to a balanced diet, regular physical activity, and smoking cessation.
Patients must also recognize the importance of consistently adhering to their prescribed therapies, as irregular medication usage can lead to negative health outcomes.
Access to healthcare services is vital, as it enables individuals to receive timely evaluations and necessary adjustments to their treatment plans.
Community health programs can offer invaluable support and education, give the power toing patients to take an active role in their health journeys and contributing to the reduction of heart-related issues.
Scroll down to read our FAQ on the survival odds for a heart attack.
Enter the captivating universe of probabilities and unique occurrences. Satisfy your curiosity by exploring our articles at WhatAreTheOddsOf.NET.